Picture this: Instead of navigating traffic and enduring stuffy waiting rooms, a patient can consult with their specialist from the comfort of their home. Or, a rural resident with limited transportation options can finally accessmental health services. This is the promise of telehealth – and at its heart lies video conferencing.
Picture this: Instead of navigating traffic and enduring stuffy waiting rooms, a patient can consult with their specialist from the comfort of their home. Or, a rural resident with limited transportation options can finally accessmental health services. This is the promise of telehealth – and at its heart lies video conferencing.
The rise of telehealth has been nothing short of meteoric. Virtual consultations are transforming healthcare delivery, driven by the pandemic and evolving patient demands. Video conferencing is the core of this transformation, facilitating face-to-face, real-time interactions that are essential for precise diagnosis and the development of trusting relationships between patients and providers.
However, when healthcare enters the digital realm, there’s one non-negotiable factor: HIPAA compliance. The Health Insurance Portability and Accountability Act (HIPAA) sets strict standards for safeguarding sensitive patient data. Failure to comply can result in hefty fines and, more importantly, erode patient trust.
So, what can you expect from this guide? Here’s a snapshot:
- Decoding HIPAA: We’ll break down HIPAA’s complexities as they specifically apply to the virtual care environment.
- Essential Tools: Discover the must-have features for a truly HIPAA-compliant video conferencing solution.
- Choosing Wisely: Learn how to evaluate vendors or decide whether building your own custom solution is the best path.
- Best Practices: Get actionable tips on maintaining compliance well beyond simply choosing the right technology.
Let’s dive in and empower you to harness the transformative potential of telehealth while keeping patient data safe and secure.
Understanding HIPAA & Its Impact on Video Conferencing
Choosing the right video conferencing platform for telehealth isn’t as simple as firing up the everyday tool you use for catching up with friends. When sensitive health information enters the picture, HIPAA casts a long shadow. It’s critical to comprehend how HIPAA regulations impact video conferencing in order to protect patient information and steer clear of expensive fines.
Let’s look at all you need to know about HIPAA and how it relates to video conferences for telemedicine. We’ll sort through the complexity to make sure you make decisions that are both legally compliant and prioritize patient privacy, from what information can be shared to the technical precautions needed.
What is HIPAA?
Let’s think of HIPAA as your healthcare data’s personal bodyguard.
Technically, HIPAA (Health Insurance Portability and Accountability Act) is a federal law passed in 1996 that specifically focuses on protecting the privacy and security of sensitive health information. HIPAA has several key components that work together to create this protective shield:
- The Privacy Rule
This rule is all about patient control. It establishes the ground rules for when and how your Protected Health Information (PHI) can be used or shared. Think of it as giving patients the right to say “yes” or “no” to the ways their health data is handled.
- The Security Rule
The Security Rule is where the technical safeguards come in. It outlines specific measures that must be put in place to protect electronic PHI (think of all your digital health records). This includes things like:
- Encryption: Scrambling data so it’s unreadable without the right key.
- Access Controls: Think of strong passwords and limit who can see what data.
- Physical Safeguards: Even the physical security of servers and devices matters.
- The Breach Notification Rule
Unfortunately, even with the best precautions, data breaches sometimes happen. The Breach Notification Rule requires that if a breach of unsecured PHI occurs, affected patients and the appropriate authorities must be notified in a timely manner.
So, what exactly is Protected Health Information (PHI)?
PHI is any health data that can identify you as an individual. This includes the obvious and the not-so-obvious:
- Basic Identifiers: Name, address, birth date, Social Security number
- Medical History: Diagnoses, treatment plans, prescriptions
- Insurance Information: Policy numbers, billing records
- Other information: Photos, voice recordings, or anything else that could pinpoint you
It’s crucial to remember that HIPAA applies not only to doctors and hospitals, but to a wide range of “covered entities” and their “business associates” who handle PHI. This could include telehealth providers, health insurance companies, IT vendors, and others.
HIPAA Requirements for Telehealth/Video Conferencing
Think of using video conferencing for telehealth as entering a high-security zone. HIPAA sets strict rules of the road to ensure patient privacy remains paramount. Let’s outline the key requirements you absolutely need to be aware of:
- End-to-End Encryption (E2EE): This is the gold standard. E2EE means your telehealth session data is scrambled while in transit and only the intended participants have the keys to unlock it. No eavesdroppers allowed!
- Secure Transmission & Storage: Data security matters at every stage. PHI must be protected both when it’s being sent over the internet (in transit) and when it’s stored on servers (at rest).
- Access Controls: It’s not just about locking out hackers. HIPAA requires strict controls on who within your organization can see what patient data, and when.
- Audit Trails: Imagine a security camera for your data. Audit trails record every time someone accesses PHI, creating accountability and helping with investigations if a breach occurs.
- Business Associate Agreements (BAAs): Since you’ll likely be using a third-party video conferencing vendor, they become what’s known as a “business associate” under HIPAA. A BAA is a legally binding contract where the vendor promises to uphold HIPAA standards in handling your PHI. Avoid using solutions without BAA.
Think of HIPAA violations as health data’s worst nightmare. The penalties can be severe, ranging from thousands to millions of dollars in fines, depending on the scale and intent of the violation. In the most extreme cases, criminal charges can even come into play. It’s not just about the money – violations tarnish your reputation and damage the essential trust between patients and providers.
Essential Features of HIPAA-Compliant Video Conferencing Solutions
Assume you’re constructing a stronghold to protect your patients’ most private information. You must use the appropriate protection mechanisms when choosing a video conferencing service that complies with HIPAA regulations. Expensive user interfaces are great, but they are insufficient for safeguarding health information.
Now let’s explore the key components that make up a genuinely safe and legal telehealth encounter.
1. End-to-End Encryption (E2EE)
End-to-end encryption (E2EE) is one of the most effective ways to protect sensitive patient data. Think of it as the digital equivalent of a secret code that only you and the intended recipient know. With E2EE, your telehealth session is scrambled from the moment it leaves the sender’s device until it reaches the receiver’s, where it’s finally unlocked for viewing.
Let’s break down why E2EE is the gold standard in data protection:
- The Middleman is Blind: Even if someone intercepts your video call mid-stream, all they see is indecipherable gibberish. This includes the video conferencing service provider themselves!
- Keys to the Kingdom: Only the participants in the conversation hold the keys to decrypt the data. This minimizes potential points of vulnerability.
- Foiling Future Snooping: Even if someone records your encrypted session, they won’t be able to crack it open later.
The E2EE Caveat
It’s important to note that popular services like Skype and the standard versions of Zoom often don’t offer true E2EE. They might encrypt data, but the service provider still technically holds the keys. For HIPAA compliance, you need to ensure your video conferencing solution specifically advertises that it uses end-to-end encryption.
2. Business Associate Agreements (BAAs)
End-to-end encryption (E2EE) is one of the most effective ways to protect sensitive patient data. Think of it as the digital equivalent of a secret code that only you and the intended recipient know. With E2EE, your telehealth session is scrambled from the moment it leaves the sender’s device until it reaches the receiver’s, where it’s finally unlocked for viewing.
Let’s break down why E2EE is the gold standard in data protection:
- The Middleman is Blind: Even if someone intercepts your video call mid-stream, all they see is indecipherable gibberish. This includes the video conferencing service provider themselves!
- Keys to the Kingdom: Only the participants in the conversation hold the keys to decrypt the data. This minimizes potential points of vulnerability.
- Foiling Future Snooping: Even if someone records your encrypted session, they won’t be able to crack it open later.
The E2EE Caveat
It’s important to note that popular services like Skype and the standard versions of Zoom often don’t offer true E2EE. They might encrypt data, but the service provider still technically holds the keys. For HIPAA compliance, you need to ensure your video conferencing solution specifically advertises that it uses end-to-end encryption.
3. Secure Data Storage and Transmission
Think of your patient data as a valuable package that needs safeguarding at every step of its journey. Protecting it requires understanding two security concepts: data-at-rest and data-in-transit.
- Data-at-Rest: This refers to data that’s sitting idle stored on a server. It needs protection through methods like:
- Strong encryption that scrambles the data and makes it unreadable without the right key.
- Secure server locations with physical safeguards (think firewalls, access controls, etc.)
- Data-in-Transit: Think of this as data on the move – streaming through video calls, or being uploaded or downloaded from the telehealth platform. It needs:
- Encryption again! This prevents interception and eavesdropping during transmission.
- Secure communication protocols to ensure data travels safely over networks.
Beyond Encryption: Other Considerations
- Server Locations: Some countries have stricter data privacy laws than others. Ideally, choose vendors storing PHI on servers situated in countries with strong patient data protection standards.
- Data Retention Policies: How long is patient data stored after a telehealth session? HIPAA has rules around this, and your vendor needs to have clear policies in place.
4. Access Controls and Audit Logs
Controlling who can access what data within your telehealth system is key to HIPAA compliance. This is where access controls and audit logs come in, acting like digital bouncers and security cameras.
Access Controls: The Gatekeepers
- User Authentication: It all starts with verifying identity. Think of strong passwords combined with multi-factor authentication (like a code sent to your phone) to make sure the person logging in is who they claim to be.
- Authorization: It’s not just about getting in the door. Authorization is about what that user can access once inside.
- Role-Based Access: A receptionist shouldn’t have the same access as a doctor! Role-based permissions mean tailoring access based on a user’s job function, upholding the principle of “least privilege.”
Audit Logs: The Evidence Trail
Imagine audit logs as an un-erasable ledger of every interaction with patient data. They should track things like:
- Who: Which user accessed the data
- What: What data was viewed, modified, or deleted
- When: Timestamps showing the exact date and time of access
- Where From: Was the access from an approved device and location?
The Importance of Audit Logs
- Deterrence: Knowing their actions are being tracked encourages users to handle PHI responsibly.
- Accountability: In the event of a suspected breach, audit logs help pinpoint what happened and who might be responsible.
- Identifying Vulnerabilities: Audit logs can reveal suspicious patterns of access that might point to weaknesses in your security system.
Choosing the Right HIPAA-Compliant Video Conferencing Solution
Making the appropriate choice in HIPAA-compliant video conferencing is not a one-size-fits-all choice. It’s similar to making a custom suit in that it must precisely match the requirements and process of your company.
This section will walk you through the decision-making process and discuss the two main options: working with a reliable vendor who offers a pre-built platform or creating your own custom solution from scratch.
1. Build vs. Buy
The allure of building your own HIPAA-compliant video conferencing solution lies in the promise of complete control. However, it’s important to go into this path with eyes wide open regarding the complexities and the commitment involved.
Considerations for the Build Route:
- Significant Development Investment: Creating a compliant solution from the ground up requires a team of skilled engineers with healthcare expertise. This means substantial initial investment of time and resources.
- Security is Paramount: HIPAA necessitates robust encryption, access controls, and other security measures. Do you have the in-house expertise to architect and continuously maintain this level of security?
- Beyond the Code: HIPAA compliance isn’t just about the technology. You’ll need to develop detailed security policies, conduct regular staff training, and be prepared for ongoing audits.
- The Agility Factor: Can your internal team swiftly respond to changes in regulatory requirements or evolving telehealth needs?
When Partnering Makes Sense:
- Speed to Market: Leveraging a pre-built, HIPAA-compliant platform from a specialized vendor can shave months or even years off your launch timeline.
- Healthcare Focus: Dedicated vendors are deeply immersed in HIPAA regulations and the intricacies of telehealth. They’ve built the security safeguards into the DNA of their platform.
- Focus on Your Core Competency: Unless you’re a software development company, outsourcing the heavy lifting of compliance allows your team to focus on delivering exceptional patient care.
- Ongoing Maintenance: Vendors handle updates, security patches, and continuous compliance monitoring, lifting a significant burden from your shoulders.
Ultimately, the build vs. buy decision boils down to your organization’s specific needs, internal resources, and appetite for risk.
2. Evaluating Vendor Solutions
Choosing a HIPAA-compliant video conferencing vendor involves asking the right questions and a healthy dose of due diligence. Let’s arm you with checklists to help you rigorously evaluate potential partners.
Technical & Security Checklist:
- Encryption: Do they explicitly state the use of end-to-end encryption? What encryption standards do they employ (e.g., AES 256-bit)?
- Access Controls: How granular are the user permissions? Do they support role-based access tailored to healthcare workflows?
- Audit Logs: What types of activities are tracked and for how long? Can you easily export logs for review?
- Data Storage: Where are servers located? What are the data retention policies?
- Incident Response: What is their breach notification procedure, and how do they work with partners to remediate the situation?
Compliance & Reputation Checklist:
- Business Associate Agreement (BAA): Are they willing to sign a BAA without hesitation?
- Certifications: Do they hold independent certifications demonstrating their commitment to security (e.g., SOC 2, HITRUST)?
- Past Breaches: No platform is immune, but have they had any significant security incidents in the past? How did they respond?
- References & Reviews: Request references from healthcare clients and seek out independent reviews. What’s the word on the street about their reliability and support?
Don’t Hesitate to Dig Deeper
Remember, you are entrusting a vendor with your patients’ most sensitive information. Be prepared to go beyond surface-level answers. Ask for detailed technical documentation and descriptions of their security practices.
Choosing a HIPAA-compliant video conferencing solution isn’t a “check-the-box” exercise. By thoughtfully evaluating vendors with these questions in mind, you can be confident you’re selecting a true partner in safeguarding patient data and delivering exceptional telehealth care.
Iotum: Your Partner for HIPAA Compliant Video Conferencing
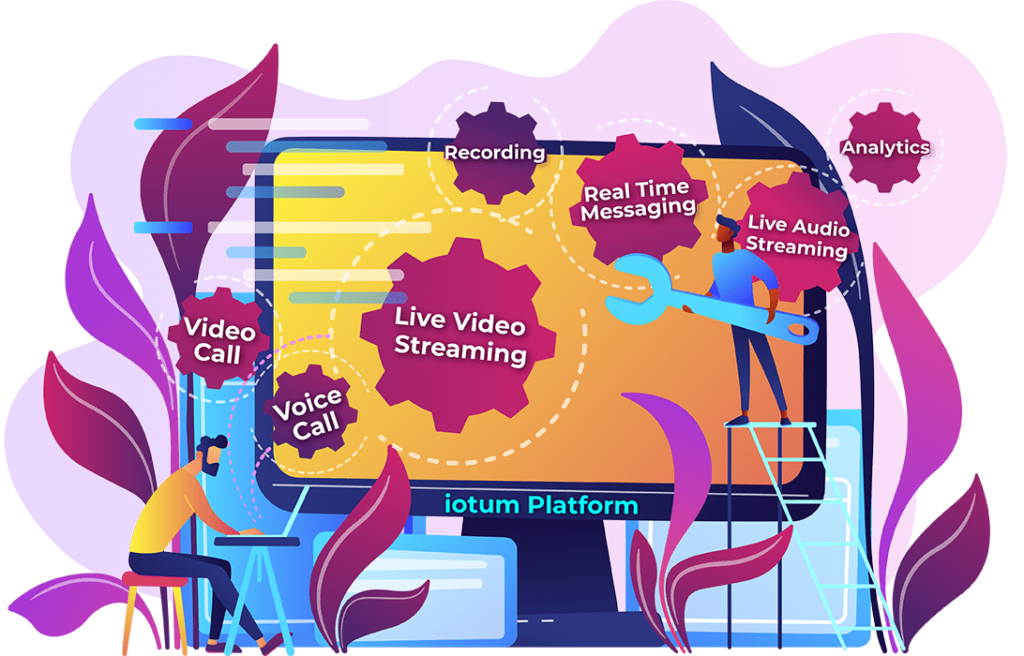
When building HIPAA-compliant telehealth experiences, having a customizable toolkit is far more powerful than a one-size-fits-all box. If you envision telehealth seamlessly blending with your unique workflows, delivering an exceptional patient experience, consider Iotum as your technology collaborator. Iotum offers HIPAA-compliant video conferencing API with a focus on safeguarding patient privacy while maintaining flexibility and reliability.
The Advantages of Custom Solutions
Think of partnering with iotum for custom HIPAA-compliant video conferencing like working with a master tailor. Instead of being forced into an ill-fitting, off-the-rack solution, we craft a solution around your specific needs. Here’s why the custom approach empowers you:
Tailored to Your Workflow
Every healthcare organization has its own rhythm and processes. Custom solutions allow you to mold video conferencing to match your unique workflows, not the other way around. For example:
- Pre-Visit Integrations: Imagine being able to have patients complete intake forms or e-consent directly within the telehealth platform, saving precious time for both staff and patients.
- Specialty-Specific Features: A dermatologist might need high-resolution image sharing capabilities, while a mental health provider might prioritize customizable virtual waiting rooms for group therapy sessions.
Seamless EHR Integration
Disjointed systems lead to inefficiencies and increase the risk of errors. With iotum, video conferencing isn’t an island. We can ensure tight integration with your Electronic Health Record (EHR), allowing for:
- Launching Telehealth Visits Directly from the EHR: No more juggling multiple systems for providers.
- Data Flow: Key information from the telehealth session can be automatically documented within the patient’s record, maintaining a comprehensive picture of their care.
The benefits of a custom approach translate into a smoother, more intuitive telehealth experience for both your providers and patients. It lets your team focus on delivering quality care, not wrestling with technology.
Iotum’s Expertise
At iotum, we understand that healthcare technology isn’t just about code, it’s about enabling better patient experiences. This vision is the basis of everything we build. Here’s why Iotum is your ideal partner for HIPAA-compliant video conferencing solutions:
Deep Roots in Healthcare
We’ve spent years developing innovative software solutions for the healthcare industry. This means Iotum understands the unique nuances of the complex regulatory environment in the healthcare landscape. We understand security best practices and streamlined workflows that are critical to delivering quality patient care. All of these considerations are woven into the fabric of our development processes.
Robust and Flexible APIs
Our API solutions are the building blocks for your custom telehealth vision. Here’s what we offer for video conferencing and beyond:
- Secure Real-Time Communication: Build crystal-clear video and audio conferencing, enabling rich interaction between patients and providers.
- Integration Capabilities: Connect your telehealth platform with EHRs, scheduling systems, patient portals – streamlining data flow and eliminating silos.
- Additional Features: We offer APIs for secure messaging, appointment scheduling, file sharing and more, so you can create a comprehensive telehealth experience.
- Customization: Our team works with you to tailor the API implementations, ensuring they seamlessly fit your specific needs.
Our Commitment to You
At iotum, we aren’t just a technology vendor, we are collaborators. We’ll be your partner through the development process while ensuring HIPAA compliance is at the forefront. We’ll walk you through each stage and give you the continuous support you require to succeed.
Best Practices for Maintaining HIPAA Compliance
Being in compliance with HIPAA requires ongoing work.Maintaining patient privacy necessitates constant attention to detail and a culture that integrates security into all facets of telehealth operations. In this section, we’ll go over best practices to help your business stay compliant in protecting patient data while also enabling your staff to provide exceptional service.
1. Staff Training
Think of your staff as the frontline defense for patient privacy. Ongoing HIPAA training is crucial to ensure everyone understands their role in keeping data safe. Here’s the why and how of effective staff training:
Why It Matters
- Human Error Factor: Most breaches, unfortunately, aren’t caused by sophisticated hackers but by well-intentioned employees making mistakes – clicking a phishing link, losing a device, etc.
- Evolving Regulations: HIPAA rules and the threat landscape aren’t static. Ongoing training keeps your team up-to-date on the latest requirements and best practices.
- Culture of Compliance: Training cultivates a shared understanding that handling PHI isn’t just a task, it’s a responsibility to uphold patient trust.
Training Beyond the Basics
- Tailored & Role-Specific: A receptionist and a physician have different levels of access and risk factors. Tailor training accordingly.
- Real-World Scenarios: Don’t just recite rules. Use case studies and examples relevant to your telehealth workflow to drive the point home.
- Make It a Habit: Regular reinforcement with short refresher sessions is more effective than one-off marathon trainings.
- Accountability: Have staff sign-off acknowledging that they understand their HIPAA obligations and the consequences of non-compliance.
2. Security Policies and Procedures
Think of your security policies and procedures as the rulebook for protecting patient data. Having them clearly written and regularly updated isn’t just about ticking a compliance box, it’s about giving your team the blueprint for handling PHI every step of the way. Here’s what your policies should address:
Technical Safeguards:
- Password Requirements: Promote strong password practices and mandate regular changes.
- Encryption Standards: Specify required encryption for data at rest and in transit.
- Access Controls: Define who can access what data under what circumstances.
- Device Management: Rules around acceptable devices (BYOD vs. organization-issued), malware protection, and remote wiping capabilities for lost or stolen devices.
Operational Safeguards
- Data Handling Practices: Procedures for secure transmission, storage, and disposal of PHI.
- Physical Security: Policies for safeguarding physical devices and limiting access to restricted areas where PHI is stored or processed.
- Incident Response Plan: A step-by-step guide for identifying, reporting, containing, and mitigating a suspected breach.
Beyond the Document
- Staff Training: Ensure everyone understands and follows the policies.
- Periodic Review: Revisit policies regularly to ensure they align with any changes in technology, regulations, or your practice’s operations.
- Enforcement: Have clear procedures for addressing policy violations, underscoring their importance.
Remember, having policies without enforcement is like having a lock without a key. By creating a clear and comprehensive set of rules, you provide a solid foundation for HIPAA compliance within your telehealth practice.
3. Regular Risk Assessments
Maintaining HIPAA compliance isn’t about achieving a static state of perfection. It requires proactive vigilance. Regular risk assessments are like having a security checkup for your telehealth systems and practices – helping catch issues before they become major problems.
Why Risk Assessments Matter:
- Identifying Hidden Vulnerabilities: Technology changes, staff turnover, even simple oversights can create cracks in your defenses. Audits reveal these weak spots.
- Evolving Threats: As cybercriminals become more sophisticated, a risk assessment helps ensure your security measures are keeping pace.
- Demonstrating Due Diligence: If a breach does occur, having documentation of regular risk assessments shows you took reasonable steps to protect patient information.
What to Look For in a Risk Assessment:
- Comprehensive Scope: Look beyond just technology. Assess physical safeguards, administrative policies, and staff awareness.
- Involve Key Stakeholders: Get input from IT, clinical staff, and leadership for a truly holistic evaluation of risk.
- Action-Oriented Findings: The goal of a risk assessment isn’t just to generate a report. It should provide an actionable roadmap for remediation and improvement.
Think of risk assessments as a long-term investment in peace of mind. By proactively identifying and mitigating risks, you keep strengthening your HIPAA compliance to maintain the trust of your patients.
Conclusion
HIPAA compliance is the foundation of trust in today’s modern healthcare procedures. For any telemedicine service, the importance of HIPAA compliance shouldn’t be neglected.
All healthcare services have a responsibility to protect patient data, and we can only fully realize the transformational potential of telehealth if we select the appropriate video-conferencing technologies, put strict security procedures in place, and promote a compliance-oriented business culture.
At Iotum, we are aware of the particular difficulties and how critical it is to create secure but patient-focused telehealth experiences. Iotum’s versatile API video conferencing solutions and HIPAA compliance experience make us the perfect partner to guide you through this challenging environment.
Let’s talk about how we may collaborate together to allow secure, compliant video conferencing for your business. Reach out to us immediately to see how we can enable you to deliver exceptional telehealth treatment while protecting the most sensitive patient data.